A concussion is a traumatic brain injury.
According to the CDC (Centers for Disease Control and Prevention)
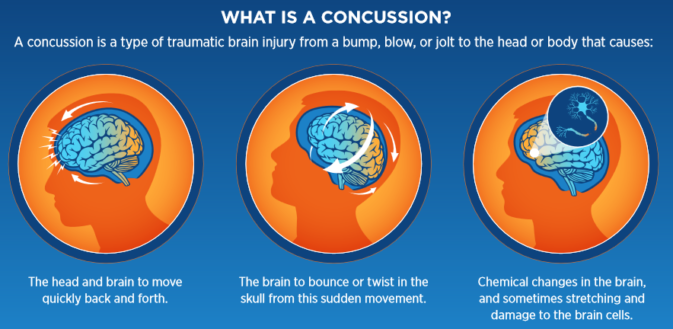
A concussion is a type of traumatic brain injury—or TBI—caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and sometimes stretching and damaging brain cells.
A concussion can also be caused by a penetrating injury (such as from a gunshot).
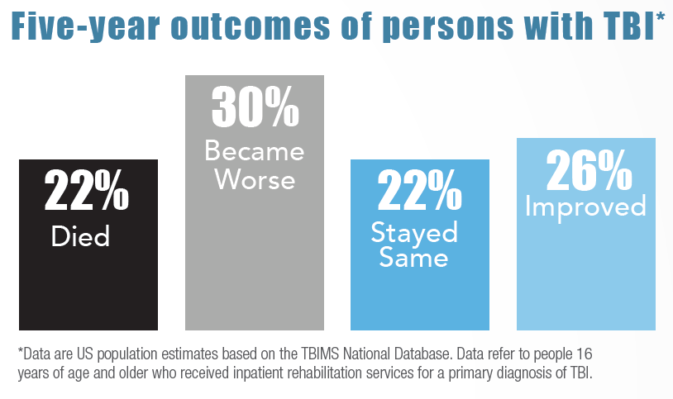
In the United States, severe Traumatic Brain Injuries (TBI) are linked to thousands of deaths each year.
another description is:
Any injury involving a bump, blow or jolt to the head or body
that results in rapid movement of the head (e.g., a sports injury, a fall, a motor vehicle accident)
A concussion can be caused by a seemingly minor accident.
Some people who have sustained a concussion may lose consciousness entirely or briefly, but not everyone does.
Symptoms of a concussion may be delayed.
They can happen immediately or take several hours or even days to present themselves.
Signs and symptoms:
Appears dazed or stunned (has a vacant stare)
Moves clumsily, balance problems or dizziness
Answers questions slowly
Inability to follow simple directions
Loses consciousness (even briefly)
Shows behavior or personality changes / mood changes like feeling sad, anxious or listless or becoming easily irritated or angry for little or no reason. Might resist treatment.
Sensitivity to light and/or noise
Hearing problems, ringing in ears (as known as tinnitus)
goes in and out of responsiveness
Headache or ‘pressure’ in head or debilitating headache
Nausea or vomiting
(Often brief) double or blurry/fuzzy vision
Feeling dinged or dazed, sluggish, hazy, foggy, or groggy
Concentration or memory problems
Confusion
Does not ‘feel right’
Can’t recall events prior to hit or fall and/or after hit or fall (see also levels of consciousness: person, place, time and event)
“A person with a concussion needs to be seen by a healthcare provider. Contact your healthcare provider as soon as you can if you think you have a concussion.”
The CDC (Centers for Disease Control and Prevention) also warns:
“In rare cases, a dangerous collection of blood (hematoma) may form on the brain after a bump, blow, or jolt to the head or body that may squeeze the brain against the skull. Call 9-1-1 right away, (if the person has) one or more of the following danger signs after a bump, blow, or jolt to the head or body.
- One pupil larger than the other
- Drowsiness or inability to wake up.
- A headache that gets worse and does not go away.
- Slurred speech, weakness, numbness, or decreased coordination.
- Repeated vomiting or nausea, convulsions or seizures (shaking or twitching).
- Unusual behavior, increased confusion, restlessness, or agitation.
- Loss of consciousness (passed out/knocked out). Even a brief loss of consciousness should be taken seriously. “
Boy Scouts list
“Mental status deterioration — from disoriented, to irritable, to combative, to coma”
in their (Boy Scouts of America Wilderness First Aid Curriculum and Doctrine Guidelines, 2017 Edition)
Brain tumor / concussion / increasing intracranial pressure from swelling or internal bleeding in the brain can cause seizures
Out in the wilderness, backpacking for example, NOLS Wilderness Medicine says
“evacuation is recommended for any patient who has become unresponsive, even for a minute or two, or who exhibits vision or balance disturbances, irritability, lethargy, or nausea and vomiting after a blow to the head regardless of whether they were knocked out. A patient who exhibits loss of responsiveness but who awakens without any other symptoms may be walked out of the wilderness with a support party capable of quickly evacuating the patient if his or her condition worsens.”
An elderly person can have a concussion from a seemingly minor fall.
Sometimes their symptoms are mistaken for a stroke.
You might not witness the fall of an elderly person,
but after the fact would notice some of the symptoms above and/or:
low-grade headache that won’t go away
having more trouble than usual remembering things, paying attention or concentrating, organizing daily tasks or making decisions or solving problems
slowness in speaking, acting, thinking or reading
getting lost or easily confused
changes in sleep patterns, inability to wake up from sleep
sensitive to light or noise
doesn’t recognize people or places
repeated vomiting
seizures (arms and legs jerk uncontrollably)
weak arms or legs, unsteady on feet
slurred speech
Note that confusion in an elderly person that comes on suddenly could be caused by a head injury
OR by a medication / improperly taking a medication,
OR by pneumonia/infection (sometimes without a fever or coughing).
The CDC (Centers for Disease Control and Prevention) notes that
“• Falls can cause head injuries. These can be very serious, especially if the person is taking certain medicines (like blood thinners). An older person who falls and hits their head should see their doctor right away to make sure they don’t have a brain injury.
• Many people who fall, even if they’re not injured, become afraid of falling. This fear may cause a person to cut down on their everyday activities. When a person is less active, they become weaker and this increases their chances of falling.”
Each year, millions of older people—those 65 and older—fall. In fact, more than one out of four older people falls each year, but less than half tell their doctor. Falling once doubles your chances of falling again.
——————————————————————-
An infant can’t answer questions or tell you they have symptoms,
but you might notice they cry persistently and it is difficult to console them,
are not interested in toys they usual are fond of (or might not even reach for a toy offered them),
have changes in eating/drinking/nursing.
They might not interact normally with a parent/sibling, give eye contact.
They might not pay their usual attention to their surroundings.
Their eyes might not follow a person/object near them, or they could even have a blank or trance-like stare.
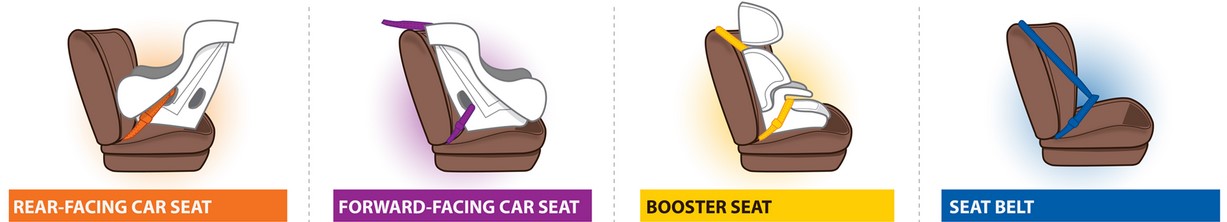
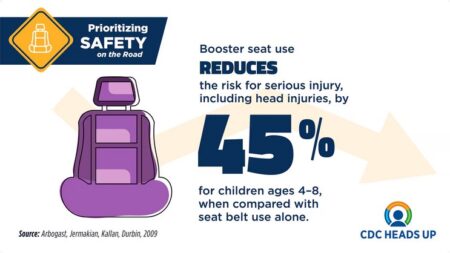
The Centers for Disease Control and Prevention (CDC) offers info on choosing the proper child seat for each age of child at:
cdctransportation.org/www.cdc.gov/transportationsafety/child_passenger_safety/index.html
——————————————————————-

Athlete who is confused about assignment or position, forgets sports plays, is unsure of game, score, or opponent.
Many teams require that an athlete with concussion symptoms be evaluated by a medical staff member with experience in the evaluation of concussions and prohibits them from returning to play on the day of the activity. Mild symptoms can resolve themselves in less than two days, but the victim still needs to be seen by a doctor.
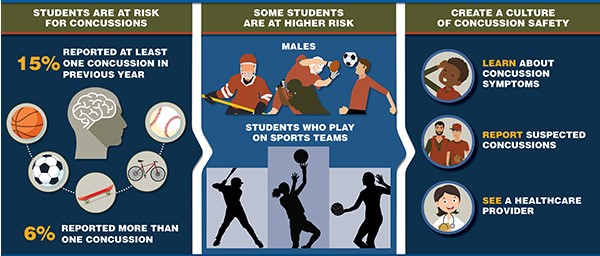
The CDC (Centers for Disease Control) notes:
“Increased susceptibility to concussions and longer recovery times among high school athletes compared with older athletes make concussions among youths playing a sport or being physically active an area of concern. Short-term and long-term sequelae of concussions can include cognitive, affective, and behavioral changes.”
For Athletes:
Clemson University gave this advice in their athletics 2017-8 Concussion Management Protocol.
“How can I prevent a concussion?
Basic steps you can take to protect yourself from concussion:
• Do not initiate contact with your head or helmet. You can still get a concussion if you are wearing a helmet.
• Avoid striking an opponent in the head. Undercutting, flying elbows, stepping on a head, checking an unprotected opponent, and sticks to the head all cause concussions.
• Follow your athletics department’s rules for safety and the rules of the sport.
• Practice good sportsmanship at all times.
• Practice and perfect the skills of the sport.
What are the symptoms of a concussion?
You can’t see a concussion, but you might notice some of the symptoms right away.
Other symptoms can show up hours or days after the injury.
Concussion symptoms include:
• Amnesia.
• Confusion.
• Headache.
• Loss of consciousness.
• Balance problems or dizziness.
• Double or fuzzy vision.
• Sensitivity to light or noise.
• Nausea (feeling that you might vomit).
• Feeling sluggish, foggy or groggy.
• Feeling unusually irritable.
• Concentration or memory problems (forgetting game plays, facts, meeting times).
• Slowed reaction time.
Exercise or activities that involve a lot of concentration, such as studying, working on the computer, or playing video games may cause concussion symptoms (such as headache or tiredness) to reappear or get worse

What should I do if I think I have a concussion?
Don’t hide it.
Tell your athletic trainer and coach
Never ignore a blow to the head. Also, tell your athletic trainer and coach if one of your teammates might have a concussion.
Sports have injury timeouts and player substitutions so that you can get checked out.
Report it.
Do not return to participation in a game, practice or other activity with symptoms. The sooner you get checked out, the sooner you may be able to return to play.
Get checked out.
Your team physician, athletic trainer, or health care professional can tell you if you have had a concussion and when you are cleared to return to play.
A concussion can affect your ability to perform everyday activities, your reaction time, balance, sleep and classroom performance.
Take time to recover.
If you have had a concussion, your brain needs time to heal. While your brain is still healing, you are much more likely to have a repeat concussion.
In rare cases, repeat concussions can cause permanent brain damage, and even death.
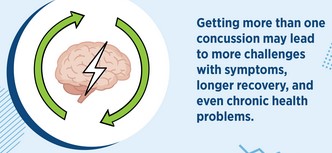
Severe brain injury can change your whole life.
It’s better to miss one game than the whole season.
When in doubt, get checked out.”

You can also search online for other Concussion Management Protocols, including at: http://www.ncaa.org/health-and-safety and https://www.cdc.gov/headsup/index.html
From Forbes:
“Many NFL players achieve success at least in part by a belief that they are invincible, or nearly so. They play the game at high speeds with near-reckless abandon, causing and experiencing impacts similar to those received in car crashes. They might not do that if they had in the back of their minds the arthritis or dementia rates of former NFL players. Acknowledgement of these risks could potentially diminish their performance. The wavering or second-guessing could therefore contribute to the end of an otherwise successful and lucrative NFL career.”
——————————————————————-
The Centers for Disease Control defines heading in soccer (or named football in other countries) as:
“using your head to stop or pass the ball”.
“UEFA (Union of European Football Associations) Heading Guidelines for youth players
The overall aim of UEFA’s Heading Guidelines is limiting the header burden in youth football to what is deemed necessary for the promotion of the game. They are intended as recommendation on how to manage heading during training and match play in youth football and how to introduce heading drills for youth players. Opinions on this matter vary from one country to another, therefore UEFA encourages National Associations to use these guidelines as a minimum and develop their specificities according to the national circumstances (such as age groups, competition organisation, club/school infrastructure, etc.).
It is acknowledged that scientific evidence at this moment does not allow for more detailed guidelines.
However, under a preventative perspective, UEFA felt that it is useful to give some practical advice though.”
The advice includes
“Ball size, ball pressure,. . .Reduce heading drills as far as possible, taking into consideration the heading exposure at matches.. . neck strengthening”
and. “Awareness for symptoms of possible concussion: If any symptoms such as dizziness, headache, unsteadiness, etc. are reported by players following heading drills, they should fully rest for at least a week, with follow-up by a medical doctor. It is noteworthy that girls are more prone to concussions and possibly also to header burden than boys.”
https://www.uefa.com/MultimediaFiles/Download/uefaorg/Medical/02/64/21/96/2642196_DOWNLOAD.pdf
——————————————————————-
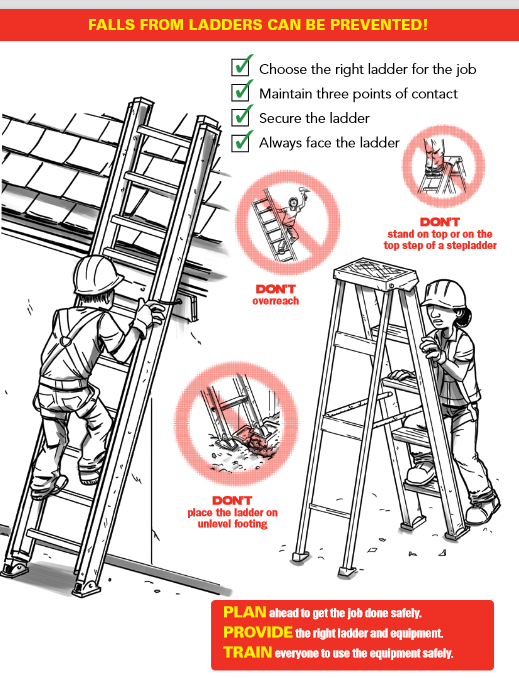
When you find someone unresponsive on the ground next to a fallen ladder and tools,
will you assume they fell and have a possible concussion / spinal injury?
OR could it be that they fell because they had a heart attack (and possibly cardiac arrest)
while on that ladder (AND have a possible concussion / spinal injury)?
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
The Centers for Disease Control and Prevention (CDC) says:
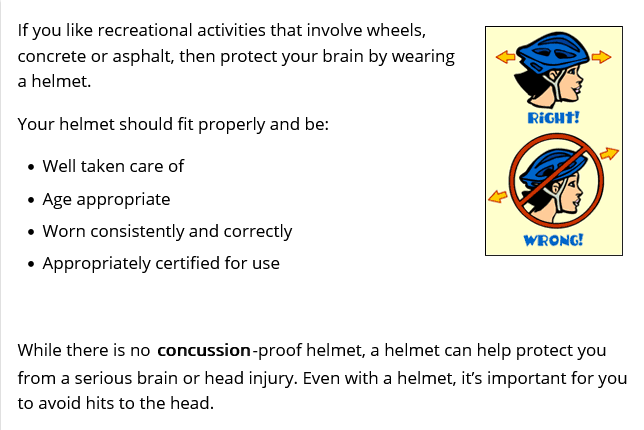
Wearing your bike helmet over a baseball cap or hat to give you shade is not advised,

and trying to fit your helmet on over the hood of your hoodie won’t work either,
the helmet needs to be firmly on your head to protect you.
And if you do paddling that requires a helmet, putting a hat with a brim on under the helmet is not advised. (Did he not tighten the helmet strap so he could fit the hat on under the helmet?)

And trying to fit your helmet on over the hood of your hoodie won’t work either.
You can get a wide brim to put over your helmet like Park Service Search and Rescue Rangers wear
(be sure to get one that does not interfere with your peripheral vision):

According to a report in the American Journal of Surgery, bike riders with helmets were less likely to die from their injuries, and less likely to break facial bones, and have 52 percent lower risk of severe traumatic brain injury.
Unfortunately, less than half of the millions of Americans who ride bicycles wear bicycle helmets. Those who do wear them are more likely to be white, female and insured.
(In Australia, Finland, New Zealand, Dubai, parts of Canada and many other places, bicycle helmets are mandatory in all states and territories for all ages.)
Many professionals wear helmets, including competitive skiers and rodeo cowboys.
Yosemite National Park Search and Rescue would like to remind you: “California law requires riders under 18 to wear helmets. Helmets are optional for bicycle riders 18 and over but they are an outstanding idea, inexpensive, and in many cases are the difference between a minor headache and life-altering or life-ending injuries. Unfortunately, when one observes bicycle operations in the Valley, the majority of adult bike riders, and even some children, opt to skip the helmet. Once the crash occurs, it’s too late to reconsider your decision to skip the helmet.”
This quote is from:
https://www.nps.gov/yose/blogs/frontcountry-biking-accident-halts-visitors-backcountry-plans.htm
Parents are often unaware that their kids
leave home wearing the bike helmet,
but then take it off and hang it from the handlebars,
often due to pressure from friends.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –

A law firm offered these reasons to wear your seatbelt
and leave a large following distance between your car and the car in front of you:
“Common Causes of Brain Injuries in Motor Vehicle Collisions
Head injuries in automobile accidents most often result from:
Direct impact against the steering wheel, dashboard, or windshield
Whiplash and impact of the brain against the inside of the skull
Ejection from the vehicle
Low-speed crashes can even produce severe traumatic brain injuries when the brain experiences rapid back-and-forth movement inside the skull.”
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
(Note to on-line users not in my classes: this is a study sheet. It is not complete instruction in first aid or the topic named in the webpage title.)
The author of this webpage, (written as a homework reading assignment for my students), does not give any warranty, expressed or implied, nor assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, product, or process included in this website or at websites linked to or from it. Users of information from this website assume all liability arising from such use.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –