Pathogens are harmful microorganisms such as bacteria and viruses, present in blood and body fluids that can cause disease in humans.
Treat all body fluids (such as diarrhea, vomit, or blood) like they are infectious.
Diseases of primary concern are Hepatitis B, Hepatitis C and HIV
as well as pathogens transmitted through the air, such as tuberculous and influenza.
Hepatitis B virus can live on a surface, exposed to the air and dried, for two weeks.
——————————————————————-
Bloodborne pathogens are spread through direct contact, indirect contact, droplet transmission and vector-borne transmission.
Direct contact occurs when infected blood or body fluids from one
person enter another person’s body at a correct entry site.
Indirect contact occurs when a person touches an object that contains
the blood or body fluid of an infected person, and that infected blood
or body fluid enters the body at a correct entry site.
Droplet transmission occurs when a person inhales droplets from an
infected person’s cough or sneeze.
Vector-borne transmission occurs when the body’s skin is penetrated
by an infectious source.
——————————————————————-
Four conditions must be met for transmission:
A pathogen is present.
There is enough of the pathogen present to cause disease.
A person is susceptible to the pathogen.
The pathogen passes through the correct entry site.
——————————————————————-
Remember this is all preventable:

Universal precautions and standard precautions:
Standard precautions you should take while providing care include:
Avoiding contact with blood and other body fluids, including saliva.
Using personal protective equipment (also referred to as PPEs), such as disposable gloves, protective eyewear, protective footwear, gowns and breathing barriers.
![]()
(Kevlar gloves are puncture resistant. Nitrile gloves are resistant to most moderate chemicals.)
Using safer equipment such as self-sheathing needles, needle-less systems or sharps with engineered sharps protection.
Disposing of sharps in proper containers.
Cleaning and disinfecting all possibly contaminated work surfaces and equipment after each use. ( Do not try to clean and re-use disposable gloves.)
(Never pour undiluted bleach straight from the bottle onto spills of blood, urine, sputum or vomit. Dangerous levels of toxic chlorine nitrous oxide gases could result.)
Avoiding touching your eyes, mouth and nose while providing care or when exposure to infectious materials is possible.
Avoid eating drinking, smoking, applying cosmetics or lip balm, or handling contact lenses while providing care or when exposure to infectious materials is possible.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Here is a drawing from the Centers for Disease Control about removing latex-free disposable gloves.
Please note that at work you will use the method your workplace says to use, which might be a little different than you learn in a first aid class.
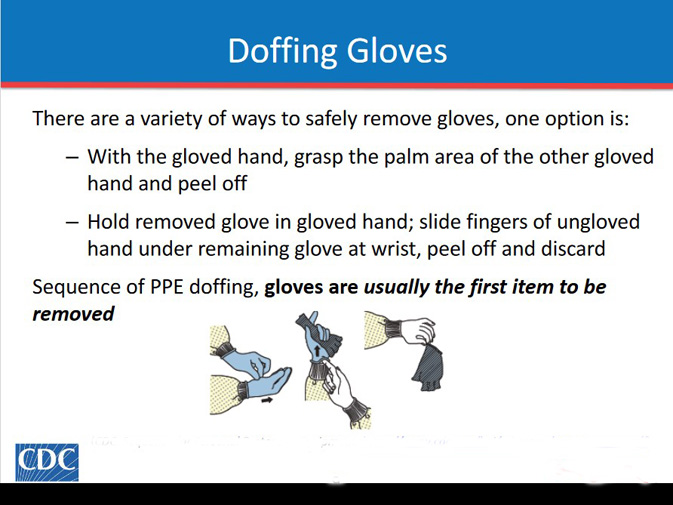
This incorrect method of removing gloves gives you (and maybe others) a risk of splashing:

– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
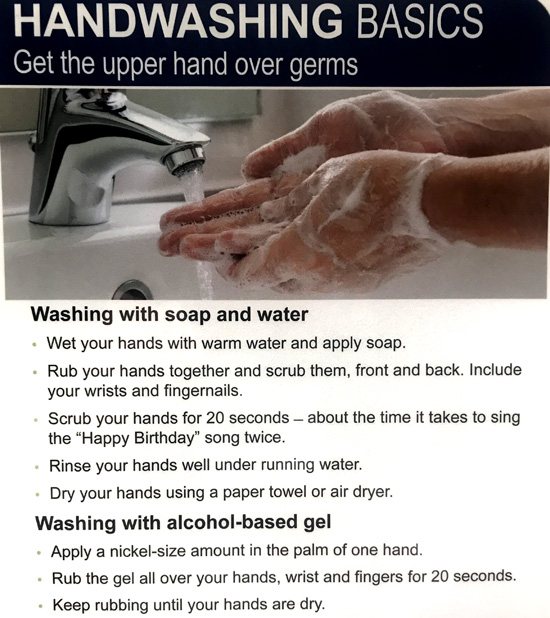
Thoroughly washing your hands with soap and warm water or other disinfectant products immediately after providing care, even if you are using disposable gloves.
Use alcohol based rubs where handwashing facilities are not available.
![]()
If you use an alcohol-based gel, a recommendation at a local hospital,
posted on the wall of the restroom, said
“apply a nickel-size amount. . .”
Remove/dispose of soiled protective clothing as soon as possible.
Disposing of contaminated materials in appropriate receptacles.
A guidelines page you might read at a faculty you work at could say:
“Disposable gloves will not be washed or decontaminated for reuse.
Utility gloves may be reused after decontamination if the integrity of the glove is not compromised. Utility gloves that are damaged in any manner or exhibit any signs of
deterioration will be discarded and replaced.” “Food and drinks will not be kept in refrigerators, freezers, shelves, cabinets, on countertops, or on benches where blood or other potentially infectious materials are present.” “Food should never be stored in refrigerators with lab specimens.” “Mouth pipetting is prohibited.”
Materials contaminated by blood include:
Items that when compressed, release blood in a liquid or semi-liquid state.
Items caked with blood that will, or may release the blood when handled.

– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
A trash bin at a restroom accessible to the public at a local hospital says on it:
DO NOT throw items with patient or confidential information in this bin.
DO NOT throw medical waste, syringes, or medical vials or anything with visible blood in this bin.
Do not throw biohazardous waste in this bin.

– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
The CDC (Centers for Disease Control and Prevention) notes:
Practicing hand hygiene is a simple yet effective way to prevent infections. Cleaning your hands can prevent the spread of germs, including those that are resistant to antibiotics and are becoming difficult, if not impossible, to treat.
On average, healthcare providers clean their hands less than half of the times they should.
On any given day, about one in 31 hospital patients
has at least one healthcare-associated infection.

The CDC says:
Follow these five steps every time you wash your hands.
Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap.
Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails.
Scrub your hands for at least 20 seconds. Need a timer? Hum the “Happy Birthday” song from beginning to end twice.
Rinse your hands well under clean, running water.
Dry your hands using a clean towel or air dry them.

AND the CDC notes that:
“These areas are most often missed by healthcare providers when using alcohol-based hand sanitizer:
• Thumbs
• Fingertips
• Between fingers”
AND the CDC has a warning about alcohol-based hand sanitizers and C.difficile:
“C. difficile is a common healthcare-associated infection that causes severe diarrhea.
C. difficile forms spores that are not killed by an alcohol-based hand sanitizer.
The spores can be transferred to patients via the hands of healthcare providers who have touched a contaminated surface or item.
If you have a C. difficile infection, make sure your healthcare providers wear gloves when examining you.
The most important way that you can prevent the spread of C. difficile is by washing your hands with soap and water after touching potentially contaminated surfaces.”
The CDC (Centers for Disease Control and Prevention) notes:
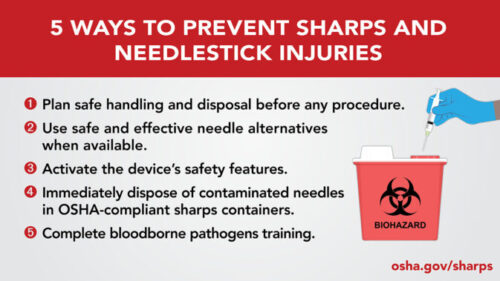
Engineering controls are the primary means of eliminating or minimizing employee exposure and include the use of safer medical devices, such as needleless devices, shielded needle devices, and plastic capillary tubes.
Best practices for preventing sharps and needlestick injuries include:
Plan safe handling and disposal before any procedure.
Use safe and effective needle alternatives when available.
Use needles with engineered sharps injury protection (SESIPs).
Always activate the device’s safety features.
Do not pass used sharps between workers.
Do not recap, shear, or break contaminated needles.
Immediately dispose of contaminated needles in in properly secured, puncture-resistant, closable, leak-proof, labeled sharps containers.
Complete Bloodborne Pathogens training.
——————————————————————-
Police are advised to “use caution when patting down a suspect.”
——————————————————————-
Exposure procedures:
Exposure incidents involve contact with blood or other potentially infectious materials.
If there is an exposure:
Clean the area of contact.
Write down what happened.
Notify your supervisor.
Immediately seek medical attention.
Follow your facility’s post-exposure policies and procedures.
______________________________________

Generally, the vaccinations you got as a child will protect you the rest of your life,
but with a few exceptions you should note.
An adult recommended vaccinations schedule
is at https://www.cdc.gov/vaccines/?CDC_AAref_Val=https://www.cdc.gov/vaccines/schedules/index.html
The CDC (Centers for Disease Control) warns: “Measles is highly contagious.
Measles can live for up to 2 hours in an airspace after an infected person leaves an area. . . . If you have measles, up to 90% of the people close to you, who are not immune, will also become infected. An infected person can spread measles to others even before knowing they have the disease. You can spread measles to others from 4 days before through 4 days after the rash appears.”
______________________________________
The HLTH57A class will cover material about administration of medications, either by assisting people with their prescriptions or by actually administering them to people. None of this will be adequate training or certification for any of you to be able to administer medications, the material in class is just for you to have an idea of what happens during administration.
At your workplace, you might get additional training to be able to administer medications, such as naloxone to a victim or patient with an overdose of opiod(s), such as fentanyl.
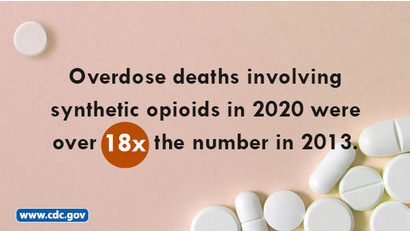
The CDC warns; “Healthcare personnel who could potentially be exposed to illicit fentanyl include nurses, nursing assistants, physicians, technicians, therapists, phlebotomists, pharmacists, students, and trainees. Healthcare personnel not directly involved in patient care, but who could be potentially be exposed to illicit fentanyl in the healthcare setting, include clerical, dietary, environmental services, laundry, security, engineering and facilities management, administrative, billing, and volunteer personnel. Possible exposure routes to illicit fentanyl vary based on the source and form of the drug. Healthcare personnel might be exposed when the patient or their personal items are contaminated with illicit fentanyl, which may be present in powder, tablet, or liquid forms. . .
The Centers for Disease Control (CDC) has videos about how to use Narcan (Naloxone) that are not required for you to watch for this class.
https://www.cdc.gov/stop-overdose/caring/naloxone.html

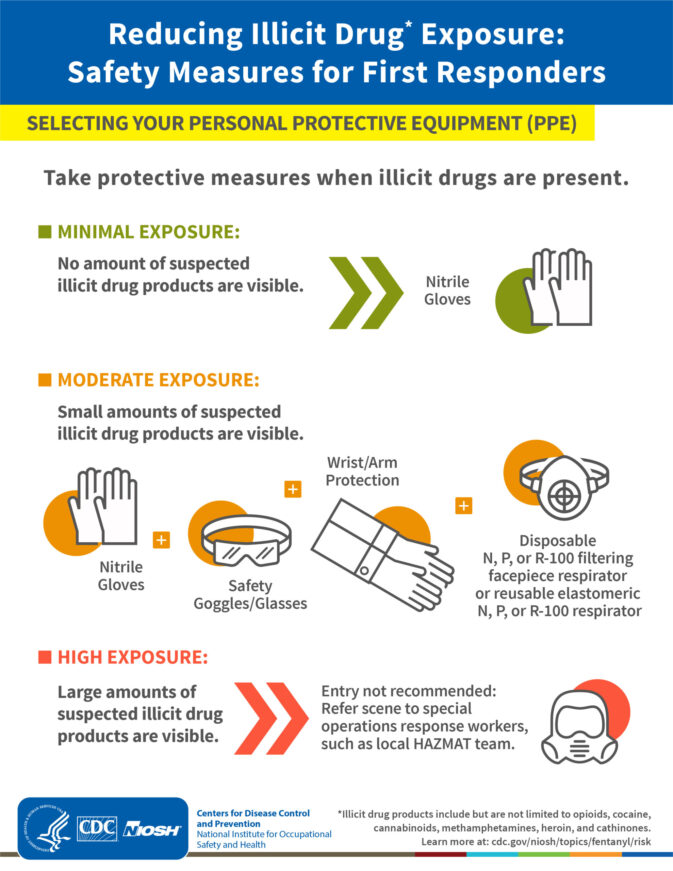
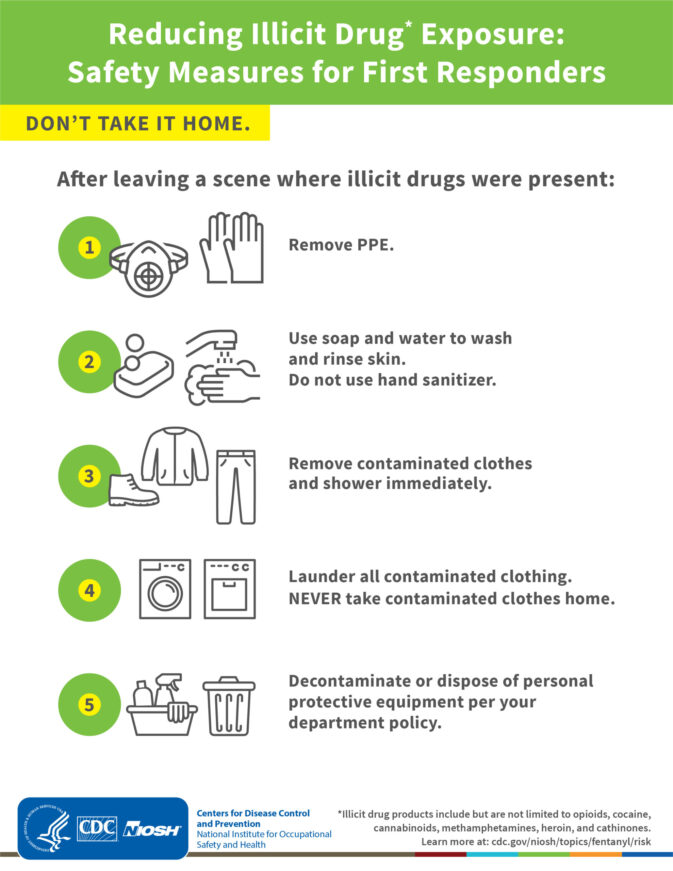
Some situations require more than the usual personal protective equipment (PPEs).
(For example, for emergency workers at natural disaster and chemical (including oil), biological, radio-logical and nuclear events, and operations specific to law enforcement, firefighting.)

A mask you commonly wear may not be enough on your face.
Please be sure you understand and follow whatever your current employer has you do.

OSHA says, in a Avian Influenza (Bird Flu) Fact Sheet
“Workplace human infections with Avian Influenza viruses do occur and everyone
with exposure to potentially infected animals needs to be aware of the exposure
risks for contracting avian flu as well as worker protection options.”
https://www.osha.gov/sites/default/files/publications/OSHA_FS-4189.pdf
Also note that the CDC says, in the case of potential exposure to illicit fentanyl
At A Minimum
“Healthcare personnel may be at increased risk of exposure to illicit fentanyl if small amounts of fentanyl products are visible on the patient, clothing, or possessions. In this case, healthcare personnel would use the following PPE:
• At least an N100, R100, or P100 disposable filtering facepiece respirator or a respirator that provides a higher level of protection
• Face and eye protection that may include goggles or a faceshield when wearing a filtering facepiece respirator
• Powder-free nitrile gloves
• Wrist/arm protection, such as sleeve covers, that would cover skin which may not be covered by usual clothing or uniform such as gowns or coveralls.”

______________________________________
and see these links about Ebola, which also requires more than the usual personal protective equipment (PPEs).
https://www.osha.gov/SLTC/ebola/
https://www.cdc.gov/vhf/ebola/index.html
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
(Note to on-line users not in my classes: this is a study sheet.
It is not complete instruction in first aid or the topic named in the webpage title.)
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
The latest on bloodborne pathogens is at: http://www.osha.gov/SLTC/bloodbornepathogens/index.html
see also:
How to pass a Red Cross written test
What the AED says as you use it
The author of this webpage, (written as a homework reading assignment for my students), does not give any warranty, expressed or implied, nor assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, product, or process included in this website or at websites linked to or from it. Users of information from this website assume all liability arising from such use.