Steps to use an AED (automated external defibrillator) are below this introduction.
This webpage can be a preview of or a review of learning to use an AED, but is not everything you would need to know to use one.
The Adult Cardiac Chain of Survival
• Early recognition of the emergency and early access to EMS
• Early cardiopulmonary resuscitation (CPR)
• Early defibrillation

• Early advanced life support
• Integrated post-cardiac arrest care
AED use by bystanders in Out Of Hospital Cardiac Arrest (OHCA) can save lives. Early CPR can help a cardiac arrest victim, but an electrical shock (defibrillation) is needed to correct the problem. The sooner the shock is administered, the greater the victim’s chance of survival.
Each minute defibrillation is delayed reduces the victim’s chance of survival by about 10 percent.
A Santa Clara County report said that 8 minutes response time from when 911 is called is the industry standard.
The Red Cross notes that “The average response time for first responders once 911 is called is 8 – 12 minutes.” And also says: “The American Red Cross supports the position that improved training and access to AEDs could save 50,000 lives each year. The Red Cross believes that all Americans should be within four minutes of an AED and someone trained to use it.”
In June, 1999, Chicago’s O’Hare Airport installed AEDs, located so that an AED was within one minute walking distance of anywhere in the airport. In the first ten months 14 cardiac arrests occurred and nine of the victims survived. That’s a 64% survival rate, compared to 3% – 4% with CPR alone.
Early CPR compressions, even hands only cpr, gets some oxygen to the victim’s brain/heart, delaying brain death and death of the heart muscle and making the heart more likely to respond properly to the use of the AED.
_______________________________________________________
Disease or injury can disrupt the heart’s electrical system.
Ventricular fibrillation (V-fib) and ventricular tachycardia (V-tach) are two of the most common treatable abnormal heart rhythms initially present in cardiac arrest victims. Ventricular fibrillation is totally disorganized electrical activity. Ventricular tachycardia is a rapid contraction of the ventricles; the heart ventricles can’t pump blood.
Defibrillation is intended to disrupt the abnormal activity of the heart, so the heart can go back to a normal rhythm and heartbeat.
Asystole is the condition when all electrical activity in the heart ceases; it can’t be corrected by defibrillation.
__________________________________________
Cardiac arrests can occur in children, most commonly due to:
- airway and breathing problems
- traumatic injuries or accidents – including motor vehicle collision, drowning, electrocution, poisoning or sudden infant death syndrome (SIDS)
- a hard blow to the chest, including hit by a baseball or in a contact sport such as hockey
- congenital heart disease
The most common cause of sudden cardiac arrest in athletes younger than 35 years is an undetected cardiac abnormality/genetic disorder.
__________________________________________
Defibrillation does not transfer any significant electrical current to a fetus, so it is safe to use on a pregnant woman.
__________________________________________
An AED (automated external defibrillator) will not shock someone who does not need it or who has a pulse.
__________________________________________
AEDs (automated external defibrillators) are easy to use, especially after you have used a model in class.
The AED talks you through what to do. You can use a make/model you have not seen before if you just look for the on/off button, perhaps a #1 button, or for some brands if you just open the AED case (lift the lid).
____________________________________________________________________
The following is quite detailed but is not complete instruction in how to use an AED. It is for my students as a preview to a class or a review after class. Trying out an AED in a class is the best way to learn to use one.
__________________________________________________________
__________________________________________________________
Steps to use an AED
Determine you need to use one, (the victim is unresponsive and not breathing) and if you do need to use the AED, get 911 or the local emergency number called.
(This has many steps and precautions I will not include here that are covered in classes.)
. . . Do not use an AED in a moving vehicle; the analysis can be affected by movement. (AND you should not be trying to transport the victim to the emergency room! Call 911 instead.)
Ideally there would be more than one person to help the victim, and one could be calling 911, while another gets the AED and another is doing CPR compressions. (If you are not familiar with CPR compressions, take a look at hands only CPR .)
______________________________________
You might need to move the victim before you can use the defibrillator:
. . . Do not defibrillate someone when around flammable or combustible materials.
(You would need to move a victim away from the pumps area at a gas station.)
. . . Remove the victim from the water (swimming pool or a rain puddle) before defibrillation.
In Red Cross instructor materials we read: “It is safe to use AEDs in all weather conditions. However, if at all possible, move the victim to a shelter to protect him or her from rain or snow, and ensure that the victim is as dry as possible. If the victim is lying in water, move him or her to a relatively dry area and wipe the chest dry before using the AED. Once you have removed the victim from the water, be sure there are no puddles of water around you, the victim or the AED. In wet weather, be sure to remove wet clothing and wipe the victim’s chest dry before placing the AED pads. Minimize delaying defibrillation when taking steps to provide for a dry environment. Different AEDs are more or less resistant to exposure to water—check the manufacturer’s instructions for specific information about the AED you will be using.”
. . . if where you are is unsafe (examples: fire is moving through a building towards you or aftershocks from an earthquake that are making the building unstable)
. . . if the victim suddenly collapsed on stairs you would have moved them to a flat surface to be able to do CPR compressions
______________________________________
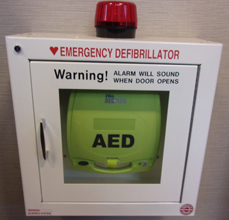
Get the AED, often from a case on a wall.
Be prepared for a loud alarm when you open the storage door on most models.
Many alarms will turn off when you shut the door after removing the AED, such as this one at the Ahwahnee Hotel (briefly named the Majestic Yosemite Hotel) in Yosemite National Park:
This at De Anza College in Cupertino, California, has a loud, high pitched alarm that does not turn off when the door is shut. (Campus police officers have a key to turn the alarm off.)
It has a warning about the alarm in big red letters:
In case of emergency, pull handle up to open, alarm will sound.
Another at De Anza College also has a loud, high pitched alarm that does not turn off when the door is shut, but no warning on the case about the alarm. (Again, campus police officers have a key to turn the alarm off.)
This AED wall storage case at the Saratoga, California, Public Library has big letters on the door:
Warning! ALARM WILL SOUND WHEN DOOR OPENS.
It also needs a key to turn off the alarm.
We do not know about any alarm at this next one.
A student (Tomoka Igari, photo below) wrote: “after taking your fun and educational CPR/AED class, I started being more aware of where AEDs are.
I am in Japan now and I found an AED in a very interesting place! … It’s installed in a vending machine!!”

In an area that is not fully open to the public, the AED might not be in a cabinet, it could be slipped into a large bracket on the wall:

or sitting on a desk, as in the office behind the front desk at Jenny Lake Lodge in Grand Teton National park:
______________________________________
If you have more than one person helping the victim, one can continue CPR compressions while the AED is being set up.
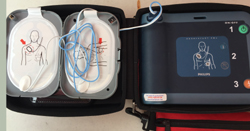
An AED might have a simple cover to open or you might need to unzip a case it is in, as these three models at De Anza:
(see a map with photos of AED locations at the college
This model the Ahwahnee hotel in Yosemite National park also has a case to unzip:
Note that the lid for the storage case often has a simple set of pictures of the steps to use the AED, and that the pads you will be applying are often in a packet in the lid (if they are not attached to the AED).

or the defibrillator itself might have photo steps to use it, along with the on / off button and the button to deliver the shock:
_________________________
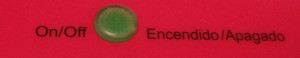
Put the AED on the floor/ground near the head/shoulders of the victim, on the opposite side of the victim from anyone doing CPR compressions, and turn on the AED.
To turn the AED on, you push the ON button, often green or yellow in color, or the button labeled number 1. (OR with some brands of AED, opening the AED turns it on automatically.)
On this model, you push the green on/off button on the upper right.
![]()
This model does not have any on/off button, it activates when you lift the lid:
_________________________
When the AED is turned on, it will start talking you through what to do.
Follow the voice prompts and/or visual prompts (some models have blinking lights for some of the steps).
Do exactly what the AED says to do, in the order the AED tells you to do things.
Some AEDs start by telling you to “get help,” “call for help,” or will have the words CALL 911 on the outside of the case to remind you to call. Other manufacturers assume you knew to call 911 or the local emergency number before you use the AED or have someone else call while you do CPR and use the AED.
It will probably not remind you to put on non-latex first aid gloves, since they are not required, but are recommended. The gloves might be in a compartment of the AED case or in a fanny pack that comes with the AED.
Most automated external defibrillators will say to remove clothing to expose a bare chest. You would need to pull the straps of a one piece woman’s swimsuit down off the shoulders and pull the suit down to her waist. Some AEDs will say to cut clothing if needed, including cutting a bra or a swimsuit bikini top and removing it from the skin (OR some bras, sports bras and swimsuit bikini tops can be lifted up and pulled up to the woman’s neck). Other AEDs say to quickly tear the clothes off; instead of slowly unbuttoning a shirt, you should pull it open and not worry about damaging the buttons! (Again, each minute defibrillation is delayed reduces the victim’s chance of survival by about 10 percent.) You might also need to move aside, but not necessarily remove, a necklace, scarf or a tie.
Sometimes scissors come with the AED, but if they did not, do not take time to go looking for scissors since the ones you use at your desk are not sharp enough to cut through clothing. Using scissors that come with the AED is also safer, since they have blunt ends. Regular scissors have sharp pointed ends that could injure the victim. Below see two pairs of scissors, one at the top of the photo with pointed ends and below it, with the yellow handle, note the blunt ends.
Some models have scissors in a fanny pack attached to the case. This model has scissors in the top of the inside of the lid of the case:
Do not use an AED on a victim wearing a nitroglycerin patch or other patch on the chest. With a gloved hand, remove any patches from the chest before attaching the device. (If your hand is not gloved you risk getting a dose of the sometimes very strong medication.) Do not try to determine if the patch is a quit smoking patch or a medication patch,
just peel it off.
Most will say to wipe the victim’s chest dry. There might be a small towel or absorbent wipes in with the AED. Sweat or other fluid on the chest can cause it to not defibrillate properly. Do not use alcohol (it’s flammable) to wipe the victim’s chest dry.
Some AEDs will tell you to clip or shave a victim’s chest if there is too much thick chest hair for the pads to stick properly. In some cases removing the first set of pads, if they did not stick properly, will also remove enough hair for a second set to stick. In Red Cross instructor materials we read: “Some men have excessive chest hair that may cause problems with AED pad-to-skin contact. Because the time to delivery of the first shock is critical, and chest hair rarely interferes with pad adhesion, attach the AED pads and analyze the heart’s rhythm as soon as possible. Press firmly on the pads to attach them to the victim’s chest. If you continue to get the “Check pads” message after removing the first set of AED pads, shave the victim’s chest and attach new pads to the victim’s chest.”
_________________________
All AEDs will ask you to attach the pads.
(If you have more than one person helping the victim, one person can continue CPR compressions while the AED pads are being put on the victim’s chest by another person.)
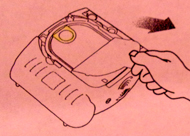
Some AEDs will just say “attach pads, plug in connector.”
– With one model we have at De Anza you will need to find the pads package (frequently in the lid of the case the AED came in) and tear open the package the pads/wiring/connector are in.
Both pads will be on the same side of the backing paper you need to peel them off of.
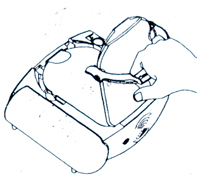
– On the model pictured below the word PULL is where you can put your fingers to open the case and remove the hard plastic cover. The drawing below the photo shows the cover easily being pulled off.
(If you forgot to turn on this AED, when you take off the lid to (open up) this compartment where the pads are, you start the defibrillator working.)
After removing the hard cover, remove a liner below it and then pull out two pads, one attached on the top and the other on the underside of a yellow plastic liner.
This model will say:
“When patient’s chest is bare, remove protective cover and take out white adhesive pads.”
IT DOES NOT TELL YOU to first look for the word PULL and first remove the hard plastic cover and then a second thinner one under the hard plastic cover. The instruction booklet that comes with the AED has a drawing of removing the thinner inner liner:
This AED model goes on to say:
“Look carefully at the pictures on the white adhesive pads.
Peel one pad from the yellow plastic liner.
Place pad exactly as shown in the picture. Press firmly to patient’s bare skin.
When the first pad is in place, look carefully at the picture on the second pad. Peel the second pad from the yellow plastic liner. Place pad exactly as shown in the picture. Press firmly to patient’s bare skin.”
The instruction booklet that comes with some models of the AED pictured above shows how to peel off the pads from the yellow plastic liner:
_________________________
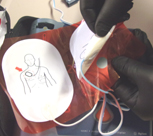
Basic rules for attaching pads common to all AEDs:
Peel each pad off the backing paper/liner before you place it.
Remove and place one pad at a time.
It does not matter which pad you put on first and which one goes on second.
The pads are usually very sticky, so watch out that your gloves don’t get stuck. (Some models have little tabs at the end of the pads to hold while you peel them off their backing so you are not as likely to get your gloves stuck on the adhesive.)
Use adult pads for adults, pediatric pads for children. If you do not have pediatric pads for a child you can use adult pads, but you can’t use pediatric pads on an adult since they will not deliver enough energy. (Local protocols on this may differ and should be followed.)
Some models may have only one size pad, and adult or child buttons to push according to the age of the victim.
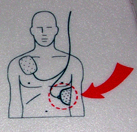
Most brands of AEDs have a map on the pads showing the correct placement of the pads:
On an adult, on all models of AEDs using two individual pads,
one always goes on the upper right of the victim’s bare chest:
and the other always goes on the lower left of the bare chest:
This is incorrect:

remember, when you are facing the victim directly, with their torso aligned the same as yours, their right side is opposite your left side.
The pads must be applied to a victim’s bare chest, with nothing between the pad and the skin.
You don’t have to remove body piercings/jewelry, but don’t put the pads over metallic body piercings/jewelry, ideally place them an inch away.
You can put AED pads on over tattoos.
You might see the outline of a pacemaker or implantable cardioverter-defibrillator under the skin. Do not place the pads directly over these medical devices, move the pad to the side.
You must press smoothly, firmly and fully to apply pads. Apply this way to not get air bubbles under the pads.
■ Some AED kits come with pediatric AED pads for use on a child up to 8 years of age or weighing less than 55 pounds (or as the manufacturer recommends).
■ Other AEDs have a button, key or switch that configures the AED for use on a child up to 8 years of age or weighing less than 55 pounds (or as the manufacturer recommends).
On a child, make sure pads are not touching. If the pads risk touching each other on a child or infant, place one in the middle of the chest and the other pad on the child or infant’s back (between the shoulder blades) the way the map on the pads shows you. Be sure the AED pads/wires on one side of them (on their back if they are lying on their back) are not touching a metal surface.
_________________________
Plug the connector at the end of the wires from the pads, into the AED, if it tells you to.
– Some models that require you to plug in a connector have a flashing light next to where the connector goes in.
The model below has a flashing light and a simple drawing of a torso with pads on it and the wires and connector heading towards where the connector needs to be plugged in.

– Some AEDs come with the wires from the pads already connected to the AED and there is no connector to plug in. (You might notice the wires already connected to the AED when you pull out the pads.) As soon as you get the pads pressed firmly on the bare chest, the AED will start analyzing.
At De Anza College we have both of these kinds of AEDs at different locations on campus.
Plugging in the connector:
On many models, (including one we have at De Anza), the connector only goes in one way. If it is turned around it will not go in:
On some models, (including one at De Anza), the connector feels as though it is pushed in when it is not.

You need to fully push in the connector.
If you do not plug/push the connector in all the way, the instructions to do so will repeat over and over again until you do: “attach pads, plug in connector,” “attach pads, plug in connector,” “attach pads, plug in connector,”
OR
“Check connector and pads,” “Check connector and pads,” “Check connector and pads.”
_________________________
If there is an ‘analyze’ button the AED will then tell you to push it, (one model will give you a “PUSH ANALYZE” voice prompt and you will see the ANALYZE LED flash), but in most models, the AED starts analyzing when you plug in the connector (or with the models that have the wires from the pads already attached to the AED, when you have firmly placed the pads on the chest).
The AED will then say “analyzing, everyone stand clear,” or “analyzing heart rhythm, don’t touch the patient,” or “no one should touch the patient, analyzing, or stand clear, analyzing now, stand clear” Make sure no one, including you, is touching the victim. Look to see that you, the person who is helping you and every bystander is not touching the victim, including a family pet. Tell everyone to stand clear. Say it in a “loud, commanding voice”. (If anyone is touching the victim while the AED is analyzing it may affect analysis.)
Do not use a mobile phone or radio within 6 feet of an AED, Electromagnetic and infrared interference generated by radio signals can disrupt analysis. (Remember to look up from what you are doing and check if, for example, a security guard might be talking on their radio and you need to remind them to move away.)
On this model, a tiny triangular button on the right just above the orange shock button will flash yellow as a reminder when you should be sure to not touch the victim.
_________________________
Let the AED analyze.
After it analyzes, it may say “shock advised, charging, stand clear,” or “preparing to shock,” and it might sound a loud beep OR a loud, high-pitched, two-tone sound or make a warbling siren-like sound. Again, you need to make everyone move clear of the victim. BUT some newer models of AEDs allow people to be doing CPR compressions while the machine charges. Do what the AED tells you to do.
A few seconds may go by between the AED saying it is doing something and the AED telling you the next step it wants you to take. These seconds can seem like a long time and I have found some of my students trying to push the shock button BEFORE they should. Wait until the AED tells you to do whatever step is next.
_________________________
If a shock is advised, look again to be sure no one is touching the victim and tell everyone again to stand clear. Say it in a “loud, commanding voice”. (If anyone is touching the victim during defibrillation, they could be shocked.) And then if the AED tells you to, “press the orange flashing button now,” OR “push the shock button” you should push the ‘shock’ button (or the #3 button). Shock delivery buttons are usually red or orange in color, with or without a lightning symbol, often flashing a light.

On the model pictured below, the shock button is the round orange one on the lower right:
_________________________
Many models will keep repeating “press the orange flashing button now,” OR “push the shock button” if it is not pushed.
_________________________
The AED might not say anything after you push the shock button or it might say:
“Stand clear. Shock will be delivered in 3 … 2 … 1 … Shock delivered.”
At De Anza, the model shown below says: “Shock delivered. It is safe to touch the patient. Begin CPR. For help with CPR, press the flashing blue button.” The round blue button in the center of the right hand side will flash when you can push it to get instructions for CPR:
_________________________
After the shock, or if no shock is indicated, the AED usually tells you to give 5 cycles of CPR (about 2 minutes) before the AED will analyze the heart rhythm again.
Some models beep at a proper rate to give the CPR compressions.
______________________________________
If the defibrillation did not work, or if no shock was advised, paramedics have some drugs that can possibly help the victim so the AED will work for them. BUT you need to have an emergency action plan, for your location, well thought through and even practiced, that will allow the paramedics to get to the victim as quickly as possible.
AND you must remember to get 911 called immediately when you have determined that the AED is needed.
You might have people stand outside your building at each side/end to wave their arms to the ambulance / fire engine as it pulls in so they know where to go. People at the end of long corridors / hallways could also hold doors open, wave and point to the staircase, or to another person at a corner of an interior hallway or the door to the room the victim is in, for example. Someone could hold the elevator on the bottom floor so it is not in use and the paramedics, their gear and the gurney can get to an upper floor faster. Someone might need to be at a narrow stairway / hallway keeping people to one side, or even telling people to keep the stairway / hallway clear for a few minutes until the paramedics can get to the victim. Have you thought through which driveway will get the ambulance closest / fastest to a particular end of a large building? Is there an exterior doorway normally locked / blocked from people using it to enter that you could have someone standing at to keep it open?
At the college, only staff / faculty should do these jobs, having students do them risks injury. For example, if a student got over-enthusiastic and walked out into traffic. Yes, campus security / police often guide fire/ambulances to locations of campus, but sometimes they might be too busy.
Do people have a rehearsed plan for what to say to the dispatcher? They should describe the emergency, as in “we have an adult who is unconscious.” If you needed to get an ambulance to the De Anza pool, it would get there faster if you could describe to the 911 operator how to find the entrance to the pool complex. This could work: “take the Stelling road entrance into the college. The pool complex entrance is at the west end of the three story parking garage.”
Does everyone in your work area who might be the one to call 911 know north / south / east / west for your location well enough to tell 911, for example, that the entrance and/or room EMS needs to get to is on the north-east corner of the building? If not, look it up on a map, show colleagues the map and talk about it. Perhaps make a map of your building to put next to each phone.
see more at: How to call 911
____________________________________
Do not remove the pads or disconnect them from the defibrillator, even if the defibrillation worked and the victim regains consciousness or even if no shock was advised. Let emergency personnel decide what to do with the pads when they arrive. (One exception would be if the defibrillator gives you instructions for a low battery, or pads that are not functional.)
(Follow the AED prompts when giving care, even if they are different from those above.) The machine might say to deliver two or three shocks, for example, instead of just one.
Always follow local protocols, manufacturers’ instructions and medical direction.
__________________________________________
A victim may gasp during CPR and/or the during preparation for use of, or during use of the AED. Agonal gasps are common in the early stages of cardiac arrest. Bystanders often report to 911 dispatchers that victims of cardiac arrest are ‘breathing’ when they have agonal gasps, as a result CPR is not given to victims who might benefit from it and an AED is not used. An irregular, gasping or shallow breath is not normal breathing and should be cared for as if the person is not breathing at all.
__________________________________________
It is possible to receive a mild shock if an implantable cardioverter-defibrillator delivers a shock to the person during CPR. The risk to responders is minimal because the amount of electrical energy involved is low.
__________________________________________
Signs and symptoms of a heart attack; a discussion of consciousness; how to do compressions-only-CPR if you witness the sudden collapse of an adult; elements of effective, quality CPR compressions, heart disease and notes on calling 911 are at hands only CPR
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
39% of European countries require CPR training
for a driving license. The European Resuscitation Council (ERC) and European Driving Schools Association (EFA are working towards mandatory CPR training for new drivers across Europe. (“Learn to Drive. Learn CPR.”,) The European Parliament has backed mandatory CPR training in its new Driving License Directive proposal.
“Cardiac arrest is a major health problem in Europe and around the world. Every year over 400,000 people in Europe and 60,000 in Italy are affected by cardiac arrest. In 70% of cases, cardiac arrest is seen by laypeople who could start cardiopulmonary resuscitation (CPR) if they knew how to do it.
The immediate initiation of CPR can double or triple survival from cardiac arrest. In fact, if witnesses of cardiac arrest start CPR before the ambulance arrives, the victims’ chances of survival increase two to three times compared to cases in which CPR is not started.”
The above was as of early 2025. See https://cprguidelines.eu/news for updates.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
__________________________________
From EMS World:
“Commotio cordis, also known as cardiac concussion, occurs when a person receives a blow to the chest during a vulnerable window during diastole of the heart. This concussive force, occurring during the upstroke of the T-wave, triggers ventricular fibrillation Sudden Cardiac Arrest. Commotio cordis can occur in both contact and noncontact sports and should be suspected anytime an athlete experiences blunt trauma to the chest followed by sudden collapse.”
How to Call 911 includes times to NOT call 911 and what to do if you call 911 by mistake.
What the AED says as you use it
How to pass a Red Cross written test
__________________________________
Perhaps also of interest:
Seizures, causes of and basic care for
Injuries Quick Facts which includes: Will this wound require stitches? and Critical Burns (you do not need to call 911 for every burn, but for critical burns you do need to call).
Choking risk factors and prevention (adults and children)
Heat Illnesses which includes warnings about dehydration.
Cold illness and injuries (hypothermia, frostbite and prevention)
At altitude which details mountain sickness (AMS), that almost everyone gets when they travel to higher-than-Silicon-Valley-elevations in any mountain range. And it has details about high-altitude cerebral edema (HACE), and high-altitude pulmonary edema (HAPE). HACE and HAPE can be fatal unless people are aware of them and ready to descend to a lower altitude.
Descending (going down to a lower elevation) is the required first aid.
Bloodborne Pathogens quick facts
First Aid for Public Safety Personnel study guide
Community Emergency Response Team training (CERT)
first aid Secondary Assessment
Times to suspect a spinal injury (symptoms, causes, signs of spinal injury)
causes of fainting, altered mental status, sudden altered mental status, unconsciousness
Seizures, causes of and basic care for
Concussion signs and symptoms, prevention
 Bloodborne Pathogens quick facts which includes an adult recommended vaccinations schedule, and areas of hands that are most often missed by healthcare providers when using alcohol-based hand sanitizer.
Bloodborne Pathogens quick facts which includes an adult recommended vaccinations schedule, and areas of hands that are most often missed by healthcare providers when using alcohol-based hand sanitizer.
__________________________________
__________________________________
From THE PHYSICIAN AND SPORTSMEDICINE:
AED Trips a Canine Alarm
(A number of years ago) . . . “Last fall, the automated external defibrillator (AED) used by the Atlanta Braves created quite a stir when the team traveled to play the New York Mets.
John D. Cantwell, MD, an Atlanta cardiologist and a team physician for the Braves, recounts how the team and all its equipment had to pass a security clearance because of controversy surrounding Braves pitcher John Rocker. (Rocker’s inflammatory comments had been widely quoted.) “Everything cleared, then our equipment started beeping, and the bomb-sniffing dogs went ballistic,” Cantwell says. “It was the AED signaling that its battery was low.”
The moral: When traveling, make sure AEDs are fully powered, especially around bomb-sniffing dogs.”
__________________________________
__________________________________
The author of this webpage, (written as a homework reading assignment for my students), does not give any warranty, expressed or implied, nor assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, product, or process included in this website or at websites linked to or from it. Users of information from this website assume all liability arising from such use.
Note to on-line users not in my classes: this is a study sheet. It is not complete instruction in CPR or the topic named in the webpage title. This webpage is not complete training and will not substitute for a class, especially not for a CPR certification class.